Good oral health and hygiene begin with clean teeth, proper dental care habits, and awareness of daily behaviours. Brushing and flossing properly from a young age helps prevent oral disease—such as cavities, gum disease, and oral cancer—as you age. Nutrition, regular teeth cleanings, and your medical history also impact your oral health standing.
Why Is Oral Health Care Important?
If you do not practice good oral hygiene, you are at a higher risk of developing serious oral conditions and diseases. These diseases include cavities, gingivitis, periodontal disease, bruxism-related conditions, cracked tooth syndrome, and more.
If your mouth is healthy, it is easier to smell, taste, chew, swallow, speak, and smile.
Common Oral Conditions
There are many oral conditions that affect both children and adults. Some conditions are minor, while others can result in more serious oral health complications over time. Common oral conditions include, but are not limited to:
Bruxism
a condition that results in excessive grinding of the teeth, typically during sleep.
Bad Breath
also called halitosis, which is characterised by chronic bad breath.
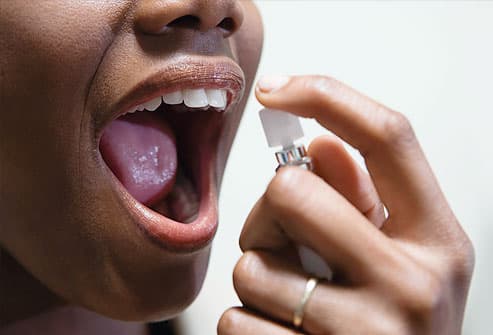
Dry Mouth
also called xerostomia, which is when the salivary glands do not produce enough saliva.
Toothaches
pain near or in a tooth, usually caused by tooth decay or an abscess.
Cracked Teeth
minor to severe cracks in teeth that are caused by an injury, bruxism, or other factors.
Tooth Sensitivity
when a tooth is sensitive to hot, cold, or sweet substances.
Temporomandibular Joint Dysfunction
a condition that results in extreme jaw pain.
Mouth Breathing
when a person regularly breathes through his or her mouth, often while sleeping.
Gum Recession
when the gums begin to wear away or pull back from the teeth, resulting in more exposure of a tooth and/or the tooth’s root.
Gingival Hyperplasia
the overgrowth of gum tissue around a patient’s teeth.
Burning Mouth
a regular burning and/or tingling sensation in the mouth.
Burning Mouth Syndrome
Burning mouth syndrome is the medical term for ongoing (chronic) or recurrent burning in the mouth without an obvious cause. This discomfort may affect the tongue, gums, lips, inside of your cheeks, roof of your mouth (palate) or widespread areas of your whole mouth. The burning sensation can be severe, as if you scalded your mouth.
Burning mouth syndrome usually appears suddenly, but it can develop gradually over time. Unfortunately, the specific cause often can’t be determined. Although that makes treatment more challenging, working closely with your health care team can help you reduce symptoms.
Symptoms
Symptoms of burning mouth syndrome may include:
- A burning or scalding sensation that most commonly affects your tongue, but may also affect your lips, gums, palate, throat or whole mouth
- A sensation of dry mouth with increased thirst
- Taste changes in your mouth, such as a bitter or metallic taste
- Loss of taste
- Tingling, stinging or numbness in your mouth
The discomfort from burning mouth syndrome typically has several different patterns. It may:
- Occur every day, with little discomfort when you wake, but become worse as the day progresses
- Start as soon as you wake up and last all day
- Come and go
Whatever pattern of mouth discomfort you have, burning mouth syndrome may last for months to years. In rare cases, symptoms may suddenly go away on their own or become less frequent. Some sensations may be temporarily relieved during eating or drinking. Burning mouth syndrome usually doesn’t cause any noticeable physical changes to your tongue or mouth.
Causes
The cause of burning mouth syndrome can be classified as either primary or secondary.
Primary burning mouth syndrome
When no clinical or lab abnormalities can be identified, the condition is called primary or idiopathic burning mouth syndrome. Some research suggests that primary burning mouth syndrome is related to problems with taste and sensory nerves of the peripheral or central nervous system.
Secondary burning mouth syndrome
Sometimes burning mouth syndrome is caused by an underlying medical condition. In these cases, it’s called secondary burning mouth syndrome.
Underlying problems that may be linked to secondary burning mouth syndrome include:
Dry mouth (xerostomia)
which can be caused by various medications, health problems, problems with salivary gland function or the side effects of cancer treatment
Other Oral Conditions
such as a fungal infection of the mouth (oral thrush), an inflammatory condition called oral lichen planus or a condition called geographic tongue that gives the tongue a map like appearance
Nutritional Deficiencies
such as a lack of iron, zinc, folate (vitamin B-9), thiamin (vitamin B-1), riboflavin (vitamin B-2), pyridoxine (vitamin B-6) and cobalamin (vitamin B-12)
Allergies or reactions to foods
food flavourings, other food additives, fragrances, dyes or dental-work substances
Reflux of stomach acid gastroesophageal reflux disease, or GERD
Stomach acid that enters your mouth from your stomach
Certain Medications
particularly high blood pressure medications
Oral Habits
such as tongue thrusting, biting the tip of the tongue and teeth grinding (bruxism)
Endocrine Disorders
such as diabetes or under active thyroid (hypothyroidism)
Excessive mouth irritation
which may result from over brushing your tongue, using abrasive toothpastes, overusing mouthwashes or having too many acidic drinks
Psychological factors
such as anxiety, depression or stress
Risk factors
Burning mouth syndrome is uncommon. However, your risk may be greater if:
- You’re a woman
- You’re perimenopausal or postmenopausal
- You’re over the age of 50
Burning mouth syndrome usually begins spontaneously, with no known triggering factor. However, certain factors may increase your risk of developing burning mouth syndrome, including:
- Recent illness
- Some chronic medical disorders such as fibromyalgia, Parkinson’s disease, autoimmune disorders and neuropathy
- Previous dental procedures
- Allergic reactions to food
- Medications
- Traumatic life events
- Stress
- Anxiety
- Depression
Complications
Complications that burning mouth syndrome may cause or be associated with are mainly related to discomfort. They include, for example:
- Difficulty falling asleep
- Difficulty eating
- Depression
- Anxiety
Prevention
There’s no known way to prevent burning mouth syndrome. But by avoiding tobacco, acidic foods, spicy foods and carbonated beverages, and excessive stress, you may be able to reduce the discomfort from burning mouth syndrome or prevent your discomfort from feeling worse.
Here are 17 Other Mouth & Tongue Problems:

Cold Sores
Also called fever blisters, you don’t get cold sores from fevers or colds but they can be triggered by them. The virus that causes cold sores is usually passed via a kiss, shared utensils, or other close contact. Over-the-counter creams and ointments may help discomfort and speed healing. Frequent sores may require a prescription. Cold sores are a top mouth problem. Other problems include canker sores, TMJ, bad breath, and mouth cancer.

Thrush
Caused by candida yeast, thrush is most common in older adults or babies. But a weakened immune system, antibiotics, diabetes, or certain medications — such as inhaled corticosteroids — can give candida a chance to grow wild. Wiping away the patches will cause soreness. See a doctor for a firm diagnosis.

Black Hairy Tongue
This painless condition occurs when the little bumps on your tongue grow long and trap bacteria that live in your mouth — making the tongue look black and hairy. Causes can include antibiotic use, poor oral hygiene, smoking, drinking a lot of tea or coffee, and not producing enough saliva. Brushing the tongue and using a tongue scraper is usually all you need to treat it, though sometimes medication is necessary.

Canker Sores
No one knows what causes these small, painful blisters inside your mouth. Triggers include hypersensitivity, infection, hormones, stress, and not getting enough of some vitamins. Also called aphthous ulcers, canker sores can show up on the tongue, cheek, even your gums. They usually last a week or two. Persistent, severe canker sores can be treated with numbing creams, prescription drugs, or dental lasers.

Leukoplakia
Leukoplakia is a reaction to an irritant, like rough teeth, badly fitting dentures, smoking, and smokeless tobacco. It can show up as white patches or plaques in the mouth, is usually painless, and can’t be scraped off. Leukoplakia can also be a precancerous condition. Persistent patches or other changes in your mouth need a dentist’s evaluation.

Lichen Planus
A rare rash that shows up as lacy, white patches or red shiny bumps on the inside of the cheeks or tongue could be lichen planus. No one knows what causes it. Generally, mild lichen planus doesn’t need any treatment. If it causes pain or ulcers, it can be treated with oral and topical medication. Oral lichen planus can be chronic and may increase the risk for oral cancer. Lichen planus can also affect skin, scalp, nails, and genitals.

Geographic Tongue
When parts of your tongue are missing some of their small bumps, you end up with raised and lowered spots, giving your tongue a map-like appearance. The spots can change location, pattern, and size within minutes to hours. Geographic tongue is harmless and can come and go. It usually doesn’t need any treatment. If there’s pain, over-the-counter pain relievers and anti-inflammatory medications can help.

Oral Cancer
A mouth sore that doesn’t go away. Unexplained numbness in the face, mouth, or neck. Problems chewing, speaking or swallowing. These are a few symptoms of oral cancer. Causes can include smoking cigarettes and using smokeless tobacco, drinking heavily, overexposure to the sun, and a family history of cancer. Oral cancer has also been linked to the human papillomavirus, or HPV. Don’t let fear keep you from the doctor — oral cancer that is caught early is treatable and curable.
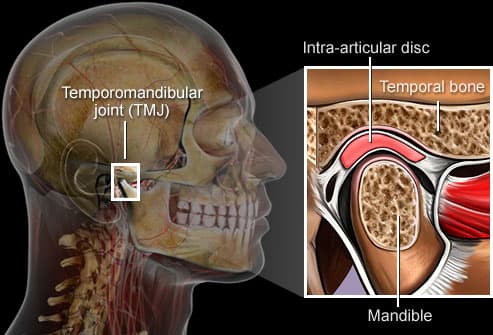
TMJ
A problem with the jaw called temporomandibular joint syndrome can cause severe pain in the jaw, face, ear, or neck. Clenching, tooth grinding, or injury can all cause TMJ syndrome, but the results are often the same: pain, headaches, dizziness, even trouble swallowing. Treatment may involve rest, moist heat, a mouth guard, medication, or surgery.

Chipped Teeth
Munching on ice or hard candies, grinding or clenching teeth, even exposing teeth to heat and cold can lead to chips, cracks, and breaks in your teeth. Tiny chips or cracks may not be a bother. But anything more could lead to pain or permanent tooth damage. Your dentist can offer dental bonding, tooth contouring, porcelain veneers, and crowns to fix badly damaged teeth.

Amalgam Tattoo
Ever notice a small blue grey “stain” in a soft part of your mouth after dental work? Called amalgam tattoos, they occur when a tiny piece of amalgam filling gets embedded in your cheek or gum. The silver in the amalgam leaches into your mouth’s soft tissue, resulting in what looks a bit like a tiny tattoo. Amalgam tattoos pose no harm. But if the blue grey spot grows or changes colour, there is a good possibility it may not be an amalgam tattoo. Ask your dentist to check it out

Gum Disease
When periodontal (gum) disease develops, bacteria in plaque accumulate along the gum line. Gingivitis is the first stage of gum disease. Symptoms include red, puffy, and bleeding gums. Proper oral hygiene can help prevent periodontal disease. Smoking, poor diet, and stress can make it worse.

Periodontitis
The next stage of gum disease is periodontitis, or gum infection. Increased inflammation causes the gums to recede, forming pockets between the teeth and gums. These pockets trap tartar, plaque, and food debris that eventually lead to infection and abscesses. Advanced gum disease damages the bone that supports teeth and is one of the leading causes of tooth loss in adults. See your dentist to treat receding gums.

Aspirin Burn
Ever let an aspirin nestle in your cheek, near an aching tooth? While you may hope this relieves pain faster, instead the acid in the aspirin burns a white, rough lesion into your gums or cheek. Preventing aspirin burn is simple — swallow those pain relievers! Treatment for aspirin burn is just as basic: Time. Simple burns should heal in about two weeks.
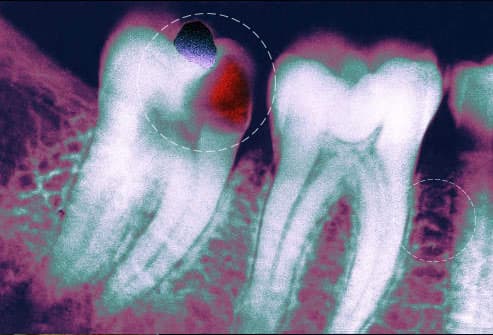
Cavities, Abscesses, Discolouration
Flossing, brushing, and rinsing daily and regular dental checkups help prevent problems like cavities, abscesses, and tooth discolouration. Don’t mess around with a severe toothache. Dental infections can spread to the face, skull, and even to the bloodstream. See your dentist as soon as possible if your tooth aches or if you have a fever, earache, or pain when you open your mouth wide.
Bad Breath
Unbrushed teeth have food particles around them that promote bacteria and cause bad breath. Persistent bad breath or a bad taste in your mouth may be from continuous breathing through your mouth, dry mouth, tooth decay, a sign of gum disease, or even diabetes. Fight bad breath by brushing your teeth and tongue, flossing and rinsing with an antiseptic mouthwash daily, drinking water, and avoiding food triggers. See your dentist if bad breath persists.

“Lie” Bumps
According to an old wives’ tale, telling a lie causes a bump on the tongue. So-called “lie bumps” or transient lingual papillitis are common even if you tell only the truth. These small, harmless bumps go away on their own after a few days, but they may be uncomfortable. Their cause is a mystery — it could be a reaction to a food or a minor trauma like biting the tongue. You don’t need to treat them, although oral anaesthetics may relieve discomfort.
How to Take Care of Your Teeth
To reduce the chance of developing a minor or serious oral condition, staying on top of basic oral care practices is essential. Many people don’t realise they may be flossing or brushing incorrectly, which can also lead to more serious problems down the road:
1. Brushing
Brushing at least twice a day is one of the most important oral care habits because it keeps the teeth and mouth healthy. Using fluoride-based toothpaste also stimulates the gums, which helps prevent gum disease and cavities.
2. Flossing
Properly flossing teeth daily helps reduce the chance of cavities forming between teeth. Flossing removes plaque and food in places where toothbrushes can’t reach. Establishing a normal routine reduces the chance of developing cavities and other oral conditions.
3. Drinking Fluoridated Water
Fluoride is a natural mineral found in soil and rocks that helps prevent cavities. Over the last 70 years, small amounts of fluoride have been added to dental materials to help strengthen tooth enamel. The mineral is naturally present in some water supplies around the United States. Fluoride is also added to many municipal water sources that have naturally low fluoride levels.
Dental Care Treatment Options
Depending on needs and the severity of an oral condition or disease, there are many different dental specialists to choose from:
General Dental Care
General dentists are the “go-to” for preventive procedures and treatments. Unlike specialists, general dentists do not specialise in one specific area of dentistry. They offer direct and indirect restorations, fillings, sealants, routine teeth cleanings, x-rays, and fluoride treatment for people of all ages.
Speciality Dental Care
Rather than providing a wide range of services, dental specialists focus on one area of dentistry. Specialists include endodontists, oral and maxillofacial surgeons, orthodontists, and periodontists.
Paediatric Dental Care
Paediatric dentists specialise in treating babies and children into adolescence. Babies should begin seeing a paediatric dentist around 1 year of age or within six months of their first tooth eruption. Doing so helps prevent baby tooth decay and cavities.
When to see a Doctor or Dentist
If you have discomfort, burning or soreness of your tongue, lips, gums or other areas of your mouth, see your doctor or dentist. They may need to work together to help pinpoint a cause and develop an effective treatment plan.
References
Website: https://www.newmouth.com/oral-health/
Website: https://www.mayoclinic.org/diseases-conditions/burning-mouth-syndrome/symptoms-causes/syc-20350911
Website: https://www.webmd.com/oral-health/ss/slideshow-tongue-your-health